How to treat Hip Bursitis

 In our central Bath clinic, our osteopaths regularly treat people with hip bursitis, or at least they have been told they have hip bursitis, either by their doctor, or they have had an MRI that shows inflammation of the bursa that lies just above the femur on their thigh. More recently research has shown that the inflammation of the bursa is secondary to changes in the tendons of the gluteal muscles that insert into the femur close to the bursa. This meant that the term hip bursitis or trochanteric bursitis was updated to be ‘greater trochanter pain syndrome’, which has now been updated again to describe the origin of the problem – gluteal tendinopathy. To successfully treat what is still commonly referred to as hip bursitis, you must address the problems that underly the problem, the changes in the tendons of the gluteal muscles that result in a tendinopathy (1).
In our central Bath clinic, our osteopaths regularly treat people with hip bursitis, or at least they have been told they have hip bursitis, either by their doctor, or they have had an MRI that shows inflammation of the bursa that lies just above the femur on their thigh. More recently research has shown that the inflammation of the bursa is secondary to changes in the tendons of the gluteal muscles that insert into the femur close to the bursa. This meant that the term hip bursitis or trochanteric bursitis was updated to be ‘greater trochanter pain syndrome’, which has now been updated again to describe the origin of the problem – gluteal tendinopathy. To successfully treat what is still commonly referred to as hip bursitis, you must address the problems that underly the problem, the changes in the tendons of the gluteal muscles that result in a tendinopathy (1).
What is a gluteal tendinopathy?
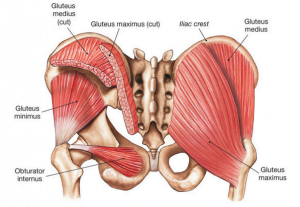 The muscles most associated with the pain are the tendons of the gluteus medius and gluteus minimus. Tendons are structures that connect muscles to bones, their job involves coping with a lot of loads when the muscle is being used, in a normal tendon, exposure to load (like a fitness routine) would strengthen the tendon and increase its ability to cope with more load. Sometimes a tendon fails to cope with the load being asked of it (either a new type of loading, or a sharp increase/decrease in load) when this happens certain changes including excessive blood vessels and, more importantly, pain nerves being deposited in the tendon that can make the tendon less able to cope with load resulting in weakness and pain when the muscle and tendon are used, this is called tendinopathy. Over time these changes mean that the tendon is more easily overloaded so even basic tasks like walking or getting up from sitting can be painful. Other factors that can also place someone at more risk of developing tendinopathy are being overweight, smoking, diabetes, or being peri-menopausal (2).
The muscles most associated with the pain are the tendons of the gluteus medius and gluteus minimus. Tendons are structures that connect muscles to bones, their job involves coping with a lot of loads when the muscle is being used, in a normal tendon, exposure to load (like a fitness routine) would strengthen the tendon and increase its ability to cope with more load. Sometimes a tendon fails to cope with the load being asked of it (either a new type of loading, or a sharp increase/decrease in load) when this happens certain changes including excessive blood vessels and, more importantly, pain nerves being deposited in the tendon that can make the tendon less able to cope with load resulting in weakness and pain when the muscle and tendon are used, this is called tendinopathy. Over time these changes mean that the tendon is more easily overloaded so even basic tasks like walking or getting up from sitting can be painful. Other factors that can also place someone at more risk of developing tendinopathy are being overweight, smoking, diabetes, or being peri-menopausal (2).
How to get rid of the pain caused by hip bursitis (gluteal tendinopathy).
The most effective way to get rid of the pain in your thigh caused by hip bursitis/gluteal tendinopathy is by combining a strategy of load management with education about the condition (3). The education portion would be making the person aware of things that may be influencing their condition, such as smoking, medications, and other lifestyle factors.
In order to get the tendon to begin to heal certain changes must be made to which loads the tendon is exposed to, in nearly all cases this means a carefully graded exercise program that will slowly increase the load on the tendon to improve its ability to cope with daily tasks, this would be coupled with advice on which activities to avoid (4).
Often it would be necessary to reduce activities that cause severe pain in the tendon, for athletes this may be very high-impact training, but for elderly people, it may be simply reducing stair or hill climbing as much as is possible until the tendon is stronger. It is also known that compression of the gluteal tendon by other nearby structures can cause pain, the highest compression force happens when the affected leg is adducted (moved towards the opposite side) so activities like crossing your legs should be avoided (5).
 One very effective exercise that has been shown to reduce the pain in the gluteal tendons for up to eight hours after completion is isometric exercises (isometric means activating the muscle but not producing any movement, see below for an example). This type of exercise will not solve the problem but they will help keep the pain at bay while you work at your recovery. What will make the most lasting change are carefully prescribed exercises that will progressively strengthen the tendon. They usually begin with exercises lying on the floor, possibly using resistance bands, and will progress up to standing and squatting exercises on one or two legs (6).
One very effective exercise that has been shown to reduce the pain in the gluteal tendons for up to eight hours after completion is isometric exercises (isometric means activating the muscle but not producing any movement, see below for an example). This type of exercise will not solve the problem but they will help keep the pain at bay while you work at your recovery. What will make the most lasting change are carefully prescribed exercises that will progressively strengthen the tendon. They usually begin with exercises lying on the floor, possibly using resistance bands, and will progress up to standing and squatting exercises on one or two legs (6).
Patient education and load management have been shown to be very effective in resolving hip bursitis, however, if this approach is unsuccessful there are other treatment options such as corticosteroid injections and surgical procedures that may also be considered (3).
If you have hip bursitis these are things you can do today to start getting out of pain –
- Get assessed by a professional such as an osteopath to ensure you get an accurate diagnosis of your pain so you can get expert advice as soon as possible.
- Reduce the duration, intensity, or frequency of activities that cause pain.
- Stop activities that may compress the bursa, such as crossing your legs.
- Sleep on the unaffected side with a pillow between your knees.
- Stop stretching the hip, especially if you are stretching the glutes and tensor fascia lata.
- Start doing some isometric exercises.
- Stop smoking.
Do you want to know what is causing your pain and if we can help? Why not take advantage of our new patient assessment introductory offer to get you started towards a tailor-made recovery plan for only £19.
Are you in a lot of pain and want to get better as soon as possible? If so then why not book in for a new patient consultation, with treatment on the day, for £75.
References
1 – Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B.(2015). Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Medicine. Aug 1;45(8):1107-19.
2 – Rees JD, Maffulli N, Cook J (2009). Management of tendinopathy. Am J Sports Med, ;37:1855-67.
3 – Reid D. The management of greater trochanteric pain syndrome: a systematic literature review. Journal of orthopaedics. 2016 Mar 1;13(1):15-28.
4 – Rio E, Kidgell D, Moseley GL, Gaida J, Docking S, Purdam C, Cook J (2016). Tendon neuroplastic training: changing the way we think about tendon rehabilitation: a narrative review. British journal of sports medicine, Feb 1;50(4):209-15.
5 – Bell-Jenje T.(2020). Greater Trochanteric Pain Syndrome – Recommended Exercises & Progressions. Part 2. Groovimovements website. Available from: https://www.groovimovements.co.za/greater-trochanteric-pain-syndrome-recommended-exercises-progressions/
6 – Grimaldi A, Fearon A (2015). Gluteal tendinopathy: integrating pathomechanics and clinical features in its management. journal of orthopaedic & sports physical therapy, Nov;45(11):910-22.

