How do you fix a lower back disc problem?

 If you have been diagnosed with a low back disc herniation you will know that it can be a very painful and debilitating condition and your thoughts have probably turned to the best and fastest way to get rid of the symptoms. Our osteopaths in Bath treat people with disc herniations almost every day. In our article below we will be explaining how best to approach the management and treatment of low back disc herniations.
If you have been diagnosed with a low back disc herniation you will know that it can be a very painful and debilitating condition and your thoughts have probably turned to the best and fastest way to get rid of the symptoms. Our osteopaths in Bath treat people with disc herniations almost every day. In our article below we will be explaining how best to approach the management and treatment of low back disc herniations.
What are the symptoms of a herniated low back disc?
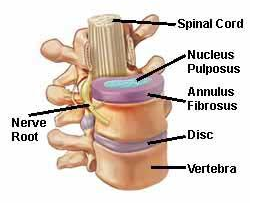
A herniated disc is commonly experienced as low back pain that ‘can be described as sharp or burning. There is often radiation of the pain in the distribution of the compressed nerve root. Numbness and tingling, as well as decreased sensation along the path of the nerve root, may also occur. In more severe cases there may be weakness or a feeling of instability while walking’ (1). Given that most low back disc herniations occur at the lower levels of the spine that are at the level of the sciatic nerve commonly the shooting pain will be felt down the back of the leg into the calf and foot (2).
 How is a low back disc herniation diagnosed?
How is a low back disc herniation diagnosed?
The diagnosis of low back disc herniation is typically made in a clinical setting by taking a full case history of the pain and how it is affected by certain movements or tasks. A set of tests are performed, such as testing the person’s reflexes and moving the person into certain postures to try to ascertain where the pain is coming from and what is causing it. A combination of the clinical history of the pain and the testing is sufficient to diagnose a low back disc herniation (2).
Do I need an MRI to diagnose a herniated disc?
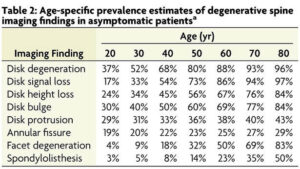
If the case history and testing do not reveal any ‘red flag’ symptoms that would indicate a serious disease or a fracture in the low back it is not recommended that people with a low back disc herniation should have an MRI. This is mainly due to the possibility of incidental findings that may result in incorrect or unnecessary treatments being applied to a person that may not affect the pain (3). People with no back pain commonly still show disc problems on imaging (see table below, 9). Back pain sufferers who receive imaging that is not wholly necessary have a higher incidence of reliance on painkillers and are more frequently recommended surgery but have higher levels of pain when followed up after one year after diagnosis (4). If, however, your pain does not improve or gets worse over the course of weeks or months then an MRI may be warranted to better understand the situation.
Does a herniated disc get better?
Yes, around 85% of people who suffer pain from acute low back disc pain will resolve in 8-12 weeks, even without treatment (1). There are also several things you can do to help with the pain and the progress of the condition.
How do I cope with the pain from a herniated disc?
The easiest and most accessible way to get on top of the pain is to take painkillers. Often if the main pain is in the low back then anti-inflammatories may be enough to make an impact on the pain. If the bulk of the pain is in the thigh and leg and is accompanied by spasms in the low back then your GP may be able to prescribe you stronger medication. It is not uncommon for the first type of medication prescribed to be ineffective, if this is the case then you should ask your GP to let you try another type as there are several options (5).
What kind of treatments work best for a low back disc herniation?
In our experience, every low back disc herniation is slightly different and no one treatment works better than another in every case.
Advice – It is highly recommended that as much as possible you should try to continue with basic daily tasks, and if the pain allows it, stay in work. This minimizes the impact that the pain will have on other aspects of your life. Ice or cold packs may also help dull the pain (6).
Exercise – Depending on the person’s symptoms they may or may not be able to do some exercise. This may take the form of advice on general activity or be more tailored to the individual’s specific needs. Often very specific stretches or positions, or strength exercises, can help reduce the pain quite quickly but each exercise needs to be carefully prescribed and taught to the person to help with their specific situation (6, 7).
 Manual Therapy – Manal treatment by an osteopath can help with reducing the symptoms of a low back disc herniation. Often these will be massage, joint mobilisation, or manipulation. Again, the choice of technique will differ with each person depending on your symptoms. Regular treatments will also help your osteopath gauge the progression of your symptoms and decide on any further action (6, 7).
Manual Therapy – Manal treatment by an osteopath can help with reducing the symptoms of a low back disc herniation. Often these will be massage, joint mobilisation, or manipulation. Again, the choice of technique will differ with each person depending on your symptoms. Regular treatments will also help your osteopath gauge the progression of your symptoms and decide on any further action (6, 7).
What if my low back disc pain does not get better?
As mentioned earlier, if your pain does not get better then further investigation may be necessary, usually beginning with an MRI of your low back. If you have tried the conservative methods described above with no progress after 4-6 months then you may be a candidate for surgery (6). The type of surgical intervention will depend on your individual situation but common options are steroid injections, microdiscectomy, or spinal nerve blocks. Surgery is considered an option of last resort as ‘Clinical data also suggest ongoing disability is an issue for some patients, with 30–70% of patients reported to experience residual pain. Recent studies also suggest that recurrent lumbar disc herniation can occur, contributing to reoperation [14% from latest figures in the UK, and can often lead to worse outcomes for patients.’ (8).
If you are suffering from pain from a low back disc then the main things to remember are;
- The vast majority of disc herniations resolve in a few months.
- You should pursue effective pain relief.
- There are several treatments and strategies that will help shorten the course of the pain, and most of these can be provided by an osteopath.
- If the situation worsens you should not delay in seeking help, either from an osteopath or your GP
Do you want to know what is causing your pain and if we can help? Why not take advantage of our new patient assessment introductory offer to get you started towards a tailor-made recovery plan for only £19.
Are you in a lot of pain and want to get better as soon as possible? If so then why not book a new patient consultation, with treatment on the day, for £75.
References
1 – Disc Herniation (2022) Stats Pesarls, National Library of Medicine. Available at; https://www.ncbi.nlm.nih.gov/books/NBK441822/
2 – Carnes, M, & Vizniak, N. (2011). Conditions Manual. Professional Health Systems, Canada.
3 – Hall A M, Aubrey-Bassler K, Thorne B, Maher C G (2021). Do not routinely offer imaging for uncomplicated low back pain BMJ; 372 :n291 doi:10.1136/bmj.n291, available at, https://www.bmj.com/content/bmj/372/bmj.n291.full.pdf
4 – Jacobs JC, Jarvik JG, Chou R, etal. Observational study of the downstream consequences of inappropriate MRI of the lumbar spine. J Gen Intern Med 2020;35:3605-12. doi: 10.1007/s11606-020-06181-7.
5 – NICE (2020). Neuropathic pain in adults: pharmacological management in non-specialist settings Clinical guideline [CG173], Published: 20 November 2013 Last updated: 22 September 2020
6 – National Spine Network (2017). National Low Back and Radicular Pain Pathway 2017, available at; https://nationalspinenetwork.co.uk/National-Back-Pain-and-Radicular-Pain-Pathway.
7 – – Van Wambeke P, Desomer A, Ailliet L, Berquin A, Demoulin C, Depreitere B, Dewachter J, Dolphens M, Forget P, Fraselle V, Hans G, Hoste D, Mahieu G, Michielsen J, Nielens H, Orban T, Parlevliet T, Simons E, Tobbackx Y, Van Schaeybroeck P, Van Zundert J, Vanderstraeten J, Vlaeyen J, Jonckheer P. (2017). Low back pain and radicular pain: assessment and management. Good Clinical Practice (GCP) Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 287. D/2017/10.273/36, available at; https://kce.fgov.be/sites/default/files/2021-11/KCE_287_Low_back_pain_Report.pdf
8 – Rushton, A., Zoulas, K., Powell, A. et al (2018). Physical prognostic factors predicting outcome following lumbar discectomy surgery: systematic review and narrative synthesis. BMC Musculoskelet Disord 19, 326. https://doi.org/10.1186/s12891-018-2240-2, available at; https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-018-22402#:~:text=Background,contributing%20to%20reoperation%20is%20reported
9 – W. Brinjikji, P.H. Luetmer, B. Comstock, B.W. Bresnahan, L.E. Chen, R.A. Deyo, S. Halabi, J.A. Turner, A.L. Avins, K. James, J.T. Wald, D.F. Kallmes and J.G. Jarvik. (2015) American Journal of Neuroradiology, 36 (4) 811-816; DOI: https://doi.org/10.3174/ajnr.A4173

 How is a low back disc herniation diagnosed?
How is a low back disc herniation diagnosed?