Current Events in Chronic Low Back Pain.
2017….nearly…..Or as we used to think of it, the future……We live in an amazing age, where technology and medical advances are changing how we live our lives with impressive speed. Sometimes advances in medicine can totally eliminate a disease or condition, more often than not treatment is targeted at relieving symptoms or arresting any progression which may cause damage to a person further down the line.
 Chronic low back pain is, unfortunately, still with us, it has (at least at time of writing) not been eradicated. It is a condition that affects 60-80% of us and is one of the most common reasons to visit a healthcare provider (1). After having an episode of low back pain one third of people will continue to have pain for up to a year, this is chronic low back pain (2). Will we ever see a time where low chronic back pain doesn’t exist? Probably not, mainly as there are so many reasons why a person may develop back pain, such as impact injuries, changes to our backs as we get older, exercise induced injuries, postural issues etc. What we can do is get better at treating low back pain when it does become chronic.
Chronic low back pain is, unfortunately, still with us, it has (at least at time of writing) not been eradicated. It is a condition that affects 60-80% of us and is one of the most common reasons to visit a healthcare provider (1). After having an episode of low back pain one third of people will continue to have pain for up to a year, this is chronic low back pain (2). Will we ever see a time where low chronic back pain doesn’t exist? Probably not, mainly as there are so many reasons why a person may develop back pain, such as impact injuries, changes to our backs as we get older, exercise induced injuries, postural issues etc. What we can do is get better at treating low back pain when it does become chronic.
Why does low back pain become chronic?
Most acute pain is a normal response telling you to react to a possibly threatening stimulus, such as a burn or a cut to your skin (3). It will reduce as the amount of damage to your body reduces. Chronic pain has been defined as ‘pain that persists for 3 months or longer……. and, while not necessarily maladaptive, often leads to physical decline, limited functional ability and emotional distress (4)’. This means that the pain can persist even though there is no obvious ‘physical’ reason for it. This can be due to a whole host of factors such as a person’s belief about the level of threat from the pain, how they have modified their activity in response to it, and if they believe it will get better or not (5).
This might sound like the dreaded ‘it’s all in your head’ response that people with chronic pain hear from friends and sometimes their doctors. Well, to a certain extent it is, at least some of the reason may be to do with the structure of your brain (although this doesn’t make the pain any less real). A recent study into low back pain found that the strongest predictor of whose low back pain went on to be chronic was the size of the areas responsible for memory and emotion. They also found that a person who experiences chronic pain will lose grey matter faster than those who don’t, meaning the brain ‘aged’ faster (6). These elements show that people may be more likely to develop chronic pain due to differences in their brain structure as well as other elements such as their beliefs and experiences to do with their pain.
 As of yet we don’t how the areas of the brain relating to emotion and memory are affecting the development of chronic pain, but there may be some insight into why the brain shows age related changes. A study in 2015 (7) looked at the impact of chronic low back pain on glial cells in the brain. Glial cells are the most common type of cell in the brain, they form a structure to support other cells, provide nutrition, repair damage and remove debris, and stimulate inflammation. The study found that sufferers of chronic low back pain had much more glial activity in the areas of the brain associated with pain. Not only that but they were able to locate the increased glial activation in the areas of the somatosensory cortex associated with the low back. They have since gone on to show a similar effect in sufferers with fibromyalgia. Previous research has shown that when the glial cells are overactive they produce chemicals that can make it easier for the nerve cells that communicate pain to produce a signal, this equals more pain (8). These very specific findings may mean that researchers may be able to produce therapies in the future designed to target these cells directly.
As of yet we don’t how the areas of the brain relating to emotion and memory are affecting the development of chronic pain, but there may be some insight into why the brain shows age related changes. A study in 2015 (7) looked at the impact of chronic low back pain on glial cells in the brain. Glial cells are the most common type of cell in the brain, they form a structure to support other cells, provide nutrition, repair damage and remove debris, and stimulate inflammation. The study found that sufferers of chronic low back pain had much more glial activity in the areas of the brain associated with pain. Not only that but they were able to locate the increased glial activation in the areas of the somatosensory cortex associated with the low back. They have since gone on to show a similar effect in sufferers with fibromyalgia. Previous research has shown that when the glial cells are overactive they produce chemicals that can make it easier for the nerve cells that communicate pain to produce a signal, this equals more pain (8). These very specific findings may mean that researchers may be able to produce therapies in the future designed to target these cells directly.
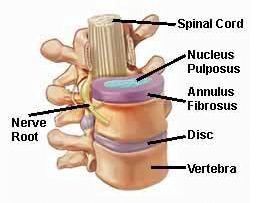
Another area of research into chronic low back pain has been looking at the possibility of some chronic back pain being caused by an infection in the intervertebral discs (9). Using this idea they recruited people who had previously suffered a low back intervertebral disc herniation and had chronic low back pain. They then injected the discs of low back pain sufferers with an antibiotic designed to resolve the bacterial infection, their results showed that 40% of the participants showed a significant improvement of their symptoms for up to a year after the course of injections. The researchers conclude that although more research is needed this type of therapy may be useful as a last resort for patients in the future.
 It is already known that outcomes for chronic low back pain sufferers are improved when a ‘multi-modal’ approach is taken (10), meaning treatment that addresses not only the physical structures of the sufferer, but also the psychological, emotional and social impact of the condition. The best hopes for the future are not that we will get rid of chronic low back pain as a condition but that we will be able to minimize its impact and duration by improving our knowledge of why it occurs, how to accurately diagnose the causes, and target an effective treatment.
It is already known that outcomes for chronic low back pain sufferers are improved when a ‘multi-modal’ approach is taken (10), meaning treatment that addresses not only the physical structures of the sufferer, but also the psychological, emotional and social impact of the condition. The best hopes for the future are not that we will get rid of chronic low back pain as a condition but that we will be able to minimize its impact and duration by improving our knowledge of why it occurs, how to accurately diagnose the causes, and target an effective treatment.
Do you struggle with chronic low back pain?
At Align Body Clinic we have helped hundreds of people who have suffered with chronic low back pain get rid of their pain and return to normal activity. We are experts in the diagnosis and treatment planning for people who have been suffering from pain for anything from a few days up to several decades. We primarily use manual therapy, medical acupuncture and carefully prescribed exercises to help people, although we also have a team of experts who can help with some of the psychological and emotional impact of long term pain.
Do you want to know what is causing your pain and if we can help? Why not take advantage of our new patient assessment introductory offer to get you started towards a tailor made recovery plan for only £19.
Are you in a lot of pain and want to get better as soon as possible? If so then why not book in for a new patient consultation, with treatment on the day, for £75.
We are also there to help you from home. Take a look at our suite of exercise resources and advice sheets which you can easily download and use from home.
References
1 – Ferreira ML, Ferreira PH, Latimer J, Herbert RD, Hodges PW, Jennings MD, Maher CG, Refshuage KM (2007). Comparison of General Exercise, Motor Control Exercise and Spinal Manipulative Therapy for Chronic Low Back Pain: A Randomized Trial. Pain; 131:31-37.
2- Chou R, Qaseem A, Snow V, Casey D, Cross TJ, Shekelle P, Owens DK (2007). Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med;147:478-491.
3 – Merskey, H. Bogduk, N. (1994). Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms, second ed. IASP Press, Seattle.
4 – Chronic Pain (2016), available at, http://www.physio-pedia.com/Chronic_Pain#cite_note-IASP-3.
5 – Magee, D. Zachazewski, J. and Quillen, W., 2009. Pathology and Intervention in Musculoskeletal Rehabilitation, Missouri, Elselvier.
6 -Baliki MN, Petre B, Torbey S, Herrmann KM, Huang L, Schnitzer TJ, Fields HL, Apkarian AV, (2012). Corticostriatal functional connectivity predicts transition to chronic back pain. Nat Neurosci. Available at, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3411898/
7 – Loggia, M. et al (2015). Evidence for brain glial activation in chronic pain patients. Brain, Mar; 138(3): 604–615.
8 –Ru-Rong, J. Temugin, B. Maiken, N. (2013). Glia and pain: Is chronic pain a gliopathy? Pain, Dec; 154(0 1): S10–S28, available at, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3858488/
9 – Albert, H. B., Sorensen, J. S., Christensen, B. S., & Manniche, C. (2013). Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. European Spine Journal, 22(4), 697–707.
10 – Samwell H, Kraaimaat F, Crul B, van Dongen R, Evers A. (2009). Multidisciplinary allocation of pain treatment: long term outcome and correlates of cognitive-behavioral processes. Journal of Musculoskeletal Pain [serial online]. March; 17(1): 26-36.
