Back Pain in Older Adults
 October 8th-12th is Back Care Awareness Week, this year their focus is back pain in older adults, so we thought we would write a quick article that focuses on how back pain affects people in later life.
October 8th-12th is Back Care Awareness Week, this year their focus is back pain in older adults, so we thought we would write a quick article that focuses on how back pain affects people in later life.
Unfortunately the incidence of back pain increases as we begin to get older, with low back pain being the most common reason that older adults have for symptoms of pain and disability (1). Also, adults aged 65 years or above, are the second most common age group to visit physicians for LBP (2). The back pain experienced by older adults can range from short term and mild to very severe and disabling, if symptoms are severe (or longstanding) enough it can lead to a loss of independence and the ability to perform daily tasks. Severe and chronic back pain has also been shown to lead to a loss of quality of life and a factor in early mortality (3).
The features of back pain also change as we age, for instance, low back pain is more common in people between the ages of 50-59, people over 70 are three times more likely to suffer from severe and chronic pain (4). Because severe back pain usually results in poor treatment outcomes and disability, timely back pain management in older adults is crucial (4).
As is common across all age groups, most back pain is mechanical and not related to disease or damage such as a fracture. This can often be referred to as ‘wear and tear’ of the back (5). There are several reasons why the incidence of back pain increases as we get older, these are mainly to do with changes in the structure of the spine and how it moves (although these changes can occur but produce no pain). These changes can be loosely described as osteoarthritis of the spine, but can also be broken down into a few different types of changes;
%27%20fill-opacity%3D%27.5%27%3E%3Cellipse%20fill%3D%22%235d6507%22%20fill-opacity%3D%22.5%22%20rx%3D%221%22%20ry%3D%221%22%20transform%3D%22rotate(169.7%2061.1%2081.6)%20scale(72.20865%20112.46457)%22%2F%3E%3Cpath%20fill%3D%22%23fff%22%20fill-opacity%3D%22.5%22%20d%3D%22M209%202.4L292.1-2l15.7%20298.4-83.1%204.4z%22%2F%3E%3Cellipse%20fill%3D%22%23fff%22%20fill-opacity%3D%22.5%22%20rx%3D%221%22%20ry%3D%221%22%20transform%3D%22matrix(-5.94193%20248.65928%20-28.548%20-.68218%2023.4%20118.4)%22%2F%3E%3Cellipse%20fill%3D%22%23fff%22%20fill-opacity%3D%22.5%22%20rx%3D%221%22%20ry%3D%221%22%20transform%3D%22matrix(27.0891%20-33.86074%20163.41202%20130.73209%20222.3%2015.6)%22%2F%3E%3C%2Fg%3E%3C%2Fsvg%3E) Intervertebral Disc Degeneration
Intervertebral Disc Degeneration
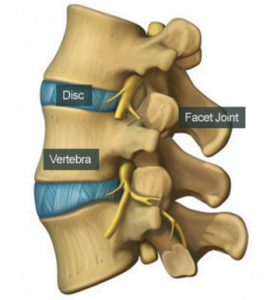
Changes to the intervertebral disc (or ‘thinning’ of the discs) in the spine is part of the aging process and can been observed in all adult age groups, getting more common in older adults. However, these changes (usually observed under MRI) are not closely linked to pain levels, and are much less likely to produce pain in older adults than in the younger population (6).
Facet Joint Pain
The facet joints are the paired joints that are on the top and bottom of each vertebra, they are part of the complex movement system of the spine. As we age, the changes in the intervertebral discs explained above result in an increased load being placed on the facet joints. This results in changes to the surfaces of the joints making them rough and un-even. This can result in localised but persistent pain in and around the affected area. These types of changes are seen in 57% of adults over the age of 65 (7).
Spinal Stenosis
As the changes to the discs and facet joints progress it can cause a condition known as spinal stenosis. These changes are more commonly seen in the elderly and are a very common reason for pain and health related disability in the more senior age groups, more so than hip or knee problems or even heart or breathing problems (8). The reason for this is mainly because the changes in the spinal bones and joints have progressed enough to cause a problem to the spinal cord, either within the spinal canal, or as a nerve exits to travel to its relevant area. When this happens there can be pain, weakness or loss of function in the limbs (most commonly the legs and feet) meaning the person can have increasing levels of disability (9).
What can you do about it?
In our clinic we commonly hear that older adults have been to the doctor with their back pain, only to be told that ‘it’s just your age, there’s nothing that can be done about it’. In severe or extremely debilitating cases surgery may be recommended but there is plenty of evidence to show that older adults can still make significant reductions in back pain and improvements to their quality of life through more conservative methods.
Painkillers
The prescription of painkillers is usually the first attempt at reducing back pain in adults, however recent research recommends that this should be a secondary option if other non-medication based therapies such as exercise and manual therapy have not been successful (14). Although some pain medications have been shown to be beneficial for certain types of back pain, for older adults they are prescribed with care and for the shortest possible time due to the possibility of side effects or interaction with other medications that are commonly taken in later life (14). Sufferers may also be offered painkilling injections, but recent guidelines suggest that these may not be effective beyond four weeks after the injection (15).
Exercise
The most important element of long term back care for the older adult is exercise, nearly all sources report that being more active will reduce levels of back pain (2, 5).  Getting an expert to do a thorough assessment and then prescribe an age appropriate programme, coupled with normal daily activity, will help reduce or prevent back pain. Most exercise will have a benefit, but the amount, type, and frequency of the exercise can make a lot of difference to results. One study found that more vigorous exercise three times a week produced an increase in low back pain, but walking and basic strength exercises reduced it (10). Most studies find that a mix of carefully prescribed stretching and strengthening exercises that are supervised will reduce back pain (2, 10, 11). Also recently highlighted as beneficial is Tai Chi movement classes, as well as helping with pain they have been shown to help with balance and leg strength (2).
Getting an expert to do a thorough assessment and then prescribe an age appropriate programme, coupled with normal daily activity, will help reduce or prevent back pain. Most exercise will have a benefit, but the amount, type, and frequency of the exercise can make a lot of difference to results. One study found that more vigorous exercise three times a week produced an increase in low back pain, but walking and basic strength exercises reduced it (10). Most studies find that a mix of carefully prescribed stretching and strengthening exercises that are supervised will reduce back pain (2, 10, 11). Also recently highlighted as beneficial is Tai Chi movement classes, as well as helping with pain they have been shown to help with balance and leg strength (2).
Manual Therapy
Getting some ‘hands on’ treatment from an expert such as an osteopath has been shown to reduce pain levels in older adults with low back pain. A mix of techniques such as stretching and manipulation of the spinal facet joints and massage, have been shown to reduce pain in the short and long term, the benefits are comparable to the use of anti-inflammatories and exercise classes (12, 13).
 For sufferers that do not seem to respond to these approaches, they may be combined to produce a more substantial benefit (16). There is also growing evidence that packages of exercise and psychological interventions, such as cognitive behavioural therapy and mindfulness, can be very helpful (14, 5).
For sufferers that do not seem to respond to these approaches, they may be combined to produce a more substantial benefit (16). There is also growing evidence that packages of exercise and psychological interventions, such as cognitive behavioural therapy and mindfulness, can be very helpful (14, 5).
What is our experience as osteopaths?
We see many older adults who have back pain, many have put up with it for years as they assume it just to do with getting older. However, many of these people can get significant reductions in their pain levels and improve their quality of life by undergoing a thorough review of their symptoms and receiving a bespoke treatment programme that will help get them moving again. Older adults usually need a more thorough assessment of their symptoms to ensure that the pain they are experiencing is coming from the back. We would also recommend that long term sufferers visit their doctor to have a review off their medications as sometimes they are taking combinations of drugs that are not helpful to their condition. You can read a more in-depth article about our treatment of older adults by clicking here.
Once we have diagnosed the issues, we can help you in a number of ways depending on what the problem is. Everything from massage, joint articulation and manipulation, to carefully prescribed exercises to help alleviate the pain. We will even give you advice on how to stop the problem reoccurring.
Do you want to know what is causing your pain and if we can help? Why not take advantage of our new patient assessment introductory offer to get you started towards a tailor made recovery plan for only £19.
Are you in a lot of pain and want to get better as soon as possible? If so then why not book in for a new patient consultation, with treatment on the day, for £75.
We are also there to help you from home. Take a look at our suite of exercise resources and advice sheets which you can easily download and use from home.
References
1 – Bressler HB, Keyes WJ, Rochon PA, Badley E. (1999). Spine, Sep 1; 24(17):1813-9.
2 – Wong, A. Y, Karppinen, J, & Samartzis, D. (2017). Low back pain in older adults: risk factors, management options and future directions. Scoliosis and Spinal Disorders, 12, 14. http://doi.org/10.1186/s13013-017-0121-3
3 – Docking, R, Fleming, J, Brayne, C, Zhao, J, Macfarlane, G, Jones, G. (2015). Sex differences, back pain and mortality. EJP, 19: 466-472. doi:10.1002/ejp.568
4 – Stewart Williams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, Wu F, Arokiasamy P, Kowal P, Chatterji S, (2015). PLoS One; 10(6):e0127880.
5 – Middleton K, Fish DE. (2009). Lumbar spondylosis: clinical presentation and treatment approaches. Curr Rev Musculoskelet Med; 2:94–104. doi: 10.1007/s12178-009-9051-x
6 – Brinjikji, W. et al (2014). Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. Available at; http://www.ajnr.org/content/36/4/811.
7 – Gellhorn, A. C., Katz, J. N., & Suri, P. (2013). Osteoarthritis of the spine: the facet joints. Nature Reviews. Rheumatology, 9(4), 216–224. http://doi.org/10.1038/nrrheum.2012.199
8 – Covaro, A., Vilà-Canet, G., de Frutos, A. G., Ubierna, M. T., Ciccolo, F., & Caceres, E. (2016). Management of degenerative lumbar spinal stenosis: an evidence-based review. EFORT Open Reviews, 1(7), 267–274. http://doi.org/10.1302/2058-5241.1.000030
9 – Genevay, S., & Atlas, S. J. (2010). Lumbar Spinal Stenosis. Best Practice & Research. Clinical Rheumatology, 24(2), 253–265. http://doi.org/10.1016/j.berh.2009.11.001
10 – Kim W, Jin YS, Lee CS, Hwang CJ, Lee SY, Chung SG, et al (2014). Relationship between the type and amount of physical activity and low back pain in Koreans aged 50 years and older. PM R; 6:893–9.
11 – Hayden JA, van Tulder MW, Tomlinson G, (2005). Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med; 142:776–85.
12 – Bromfort G, Haas M, Evans RL, et al (2004). Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine,, 4;4(3):335–56.
13 – Van Tulder MW, Koes B, Malmivaara (2006). Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J, ;15(1):S64–81.
14 – Prof Nadine E Foster, DPhil, Prof Johannes R Anema, PhD, Dan Cherkin, PhD, Prof Roger Chou, PhD, Prof Steven P Cohen, MD, Prof Douglas P Gross, PhD et al, (2018). Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet, vol 391, issue 10137, p2368-2383.
15 – Qaseem A, Wilt TJ, McLean RM, Forciea MA, (20117). Clinical Guidelines. Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med, 166: 514−30.
16 – Hayden JA, van Tulder MW, Tomlinson G (2005). Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med; 142:776–85.

 Intervertebral Disc Degeneration
Intervertebral Disc Degeneration